Thanks to everyone who submitted questions! You really got me thinking!
If you could give up one of your treatments/therapies/CF-related routines for a week, which one would it be?
I can only choose one? 😉 The treatment that I struggle with most is the breathing treatment and respiratory therapy that I do before bed, so I’d give that up for a week if I could do it without consequences. My morning treatment is actually harder because I’m far more congested first thing in the morning, but that one is so necessary for me to function that I never hesitate to do it. The instant gratification of being able to breathe and walk around without massive coughing fits is pretty motivating.
The evening treatment, on the other hand, is such a drag. I work four evenings during the week and my last students leave at either 8:30 or 9:00 pm. After that I’m pretty beat and I just want to relax, watch TV, spend time with Jaime, or go to bed. I hate having to initiate coughing and get my lungs all hot and bothered. Sometimes if I get coughing too hard, it’s difficult to stop and get to sleep.
If I miss the evening treatment, I still sleep just as well. But if I skip it, I have a harder time the next morning with more congestion and extra coughing. So there is a reward for doing it, but it’s not until the next morning. Honestly, sometimes I’m just too tired to care that I’m going to pay for it the next day.
Are there are new CF medications or treatments that might help your lung function?
I think a little background information is helpful in answering this question. As far as medications and treatments for CF, there are five main categories. The great news is that thanks to the Cystic Fibrosis Foundation, all five categories are under research and new drugs and therapies are being tested and developed!
The first category is nutritional. I currently take digestive enzymes and CF-tailored vitamins to meet my nutritional needs. Because I am stable in this area, I don’t think any of the medications under development would be of great help to me. The next area is anti-infectives which include antibiotics. Most of the research is focusing on inhaled antibiotics which go straight to the lungs. Because of my significant asthma component, I cannot tolerate any of the inhaled antibiotics that are currently available, so I don’t have much hope that new ones will help me either.
The third category is anti-inflammatory drugs. I am particularly excited about this area of research because the asthma component of my CF causes a great deal of lung inflammation. There are currently five medications in the drug development pipeline. I truly hope one of them is a winner and will help me! The fourth category is mucus clearance which includes medications to thin the mucus and devices to help us loosen the congestion and cough it out. I currently inhale saline solution and a mucus thinner and blow in a device that vibrates my lungs. My mucus is still quite thick, however, so I’m excited that there are five drugs in the development pipeline and hope that one will turn out to be more effective than what I currently take.
The fifth and most exciting category is drugs that restore CFTR function. The symptoms of CF are caused by a faulty protein which is known at the CF Transmembrane Conductance Regulator (CFTR). These drugs are designed to correct the defective protein. The defective protein inhibits sodium and chloride from moving in out and of the cells properly. There are many CF mutations and different types of mutations cause the protein to malfunction in different ways. There are currently two medications available to patients that help fix CFTR function. One medication has been particularly effective and patients who can take it have seen some significant gains in lung function and overall health. The second one has had more modest results but has still been very helpful to many patients. Due to my specific mutations, neither drug is effective for me (or available to me). I have one copy of the most common CF mutation and one rare mutation. Because I do have one common mutation there is still a good chance that there may soon be a drug in this category that will help me. I’m hoping!
If this topic sparked your interest, check out the Cystic Fibrosis Foundation’s Drug Development Pipeline for more information.
Would you ever consider a lung transplant?
The short answer is yes, I would consider it. But at this time I don’t feel certain that I would decide to go for it. My CF care team has never broached the subject with me because thankfully, at this time, I am functioning well even with diseased lungs. However, I have read some about the process and “know” people through online support groups who have gone through transplantation.
My understanding is that survival rates for patients who receive lung transplants are rising, but lungs are still a difficult organ to transplant. According to the Cystic Fibrosis Foundation, 80% of patients who receive a lung transplant are still alive after one year, and about 50% are still alive after five years. The wonderful thing about transplant is that the new lungs will never have cystic fibrosis! However the rest of the body still does, so lung transplants are not cures. Also, transplantation can cause other problems. I’ve heard people say that when you have a transplant you trade one set of issues for another. First off, transplant surgery is a major operation and there are inherent risks there. As someone who has had two major surgeries and three minor ones, the thought of the surgery itself is more than a little frightening. Patients require 24-hour-a-day care for at least a month after the procedure and most centers require at least three family members or friends to sign up to be caretakers. It is also very expensive. It would be a lot to put my family through.
In addition, patients are always at risk for rejection, which is where the body attacks the new lungs as a foreign invader. Severe rejection can lead to lung failure. Because of this, transplant patients must take many strong medications to fight against rejection. Those medications can cause other complications such as cancer, recurrent infections, kidney infection, or diabetes.
I feel there are emotional implications as well. I haven’t studied this or talked to other transplant patients about it, but the thought of receiving the lungs of someone who has died a tragic death is a little hard for me. I wouldn’t feel right about praying for new lungs or hoping to get the transplant call just knowing that what I’m ultimately waiting for is someone’s untimely demise. That said, I can imagine that the gift of organ donation might be a positive thing for the grieving family, and that blessing someone else with life from that tragedy might be a healing experience. I haven’t worked it all out in my mind, but these are my preliminary thoughts.
I’ve just listed a lot of negatives about lung transplantation, but the whole reason I would consider it is that when it is successful, it can add wonderful, healthy years to people’s lives! What a gift that would be. Some lung transplant recipients go on to become athletes or climb mountains or do all sorts of things they could never even attempt before. That sounds pretty great to me. Also, there comes a point in most CF patient’s lives where transplant is the only remaining option for treatment. If that time comes for me, I feel confident that God will show me the path to take.
What’s one really hard thing about having CF that most people don’t know about?
Great question and a hard one!! I can’t decide between two things so I’m going to cheat and write about both. The first may better answer the “most people don’t know about” part of the question, and the second better answers the “really hard thing” part.
I hesitated to write about this at first because it’s kind of dark and depressing. But I’m trying to raise CF awareness, so here’s the honest truth. The first thing that came to mind is moments of panic. I have some pretty specific fearful thoughts that come into my mind. I’m not talking about the more obvious fears of an uncertain future or fears of getting sick. These are different. Sometimes I imagine that I will need to flee from something or someone and I can’t get away because I can’t breathe well enough to run fast. I wonder what would happen if I was kidnapped or ended up imprisoned for some reason. How long would it take me to die a miserable death without access to my medications?
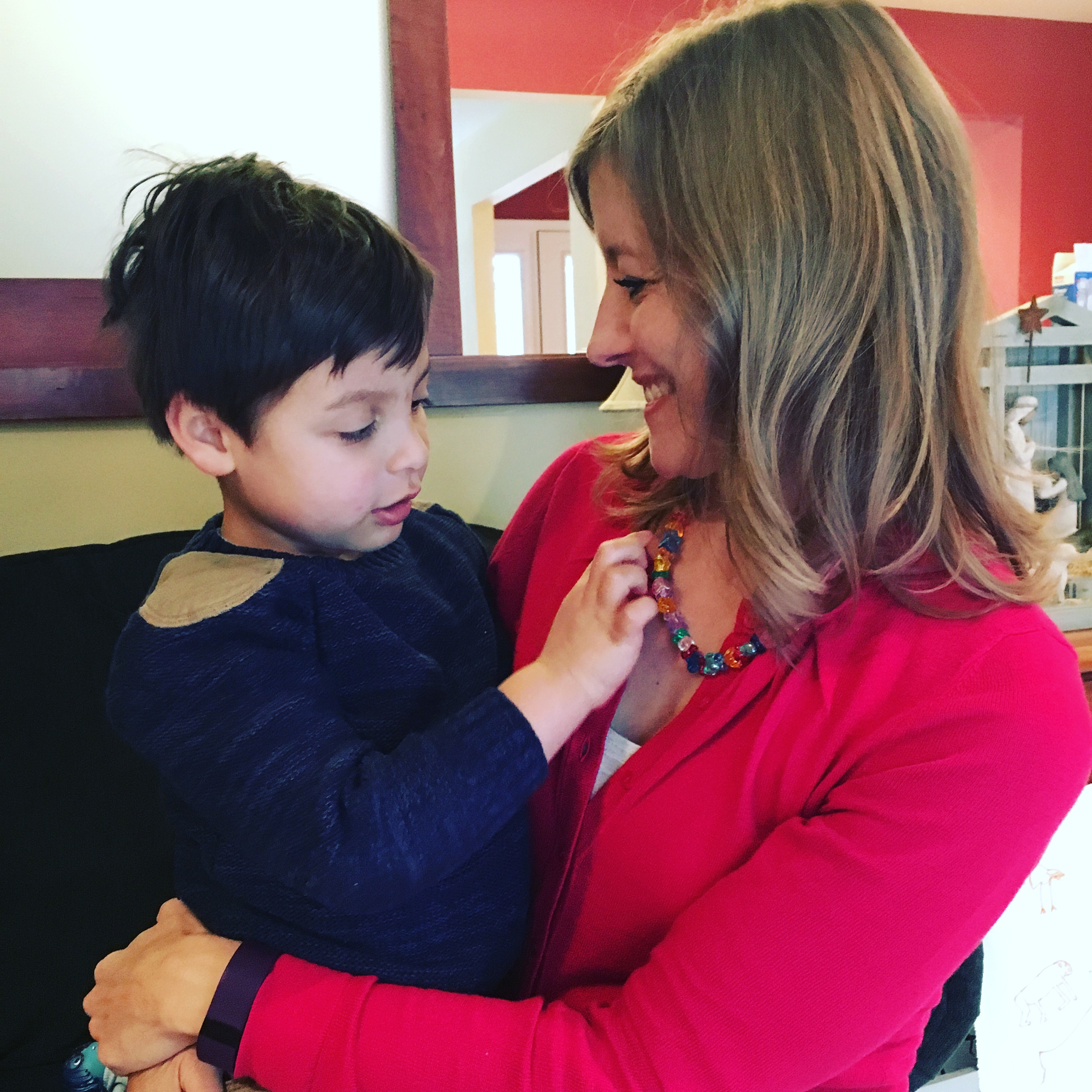
I have fears of being overpowered. I’m afraid of suffocating or being stuck in tight places. I’m scared of being buried alive in sand or snow. I can hardly stand to hang out in a blanket fort with Lucas or hide under the covers with him because after a few minutes, I feel smothered. I even hate to wear protective face masks because any sort of breathing obstruction makes me nervous and uncomfortable. I’m afraid I’ll need to rescue Lucas from something horrible and I won’t get to him in time. Now that my lung function is reduced, I don’t like having my face and head under water. I’m afraid of drowning.
When these thoughts or fears come to me during the day, it’s not hard for me to push them away and think about other things. But they also come in vivid dreams, and those can be downright terrifying. I have a recurring dream where I am unable to move, chained by some invisible force. There have been a few times in my life where I have been sick enough that I thought I was going to die for lack of breath during or after a bad coughing fit. It’s an awful feeling and I started having these fears and dreams after those experiences.
Even though I hate that part of the disease, it’s not as hard as other aspects because it’s not a constant problem. Which leads me to my second answer. I’m not sure people understand how often those of us with cystic fibrosis deal with change and loss, and how lonely that can make us feel. Because CF is a progressive disease, symptoms get worse over time. It may be obvious that we have to deal with more sick days, more coughing, more infections, and reduced lung function, but the resulting losses are more subtle. The sicker we become, the less we can do, and over time it feels like we are losing bits and pieces of ourselves along the way.
There are a whole host of things I did in my younger, healthier years that I can’t even attempt now. Some of them I have a wistful longing for–like being able to run the 8-mile race around the perimeter of Mackinac Island, or run down the side of a sand dune. Some of them are simple and seemingly trivial…like helping someone move furniture. But both were a part of my identity that I lost. Betsy the runner is gone. Betsy, that girl who’s surprisingly strong for her size and who will pitch in and help with whatever–the one who enjoys a physical challenge–she’s gone too. That hurts. It’s really hard. Sometimes these changes happen slowly over time, and sometimes they come fast and furiously. At times I haven’t even had time to accept and adjust to my new limitations before I’m faced with a whole set to get used to.
These losses happen to everyone as they age, but when you have a disease like CF, it begins far too early and only to you. Your peers aren’t going through it. When you’re facing these things together, there’s a camaraderie, maybe even humor to be found in the situation. But it’s just painful when you’re experiencing losses alone. Because of the dangers of sharing germs, cystic fibrosis patients are not permitted to mingle. There are no face to face meetings or support groups. Any support we seek has to be online. The online groups are wonderful, but it’s not the same as having a friend to share life with. It’s different to chat online than to talk face to face over coffee, or laugh (and therefore cough) during a playdate at the park with our kids. Sometimes I think it would feel really good just to get a hug from someone who really understands. I am blessed with so many wonderful, true friends and a family that loves me and helps me to bear my burdens, but at times I still feel alone in my world of disease.
How is your Fitbit streak going?
It’s going great! Today will be my 300th day in a row of 10,000 steps or more (assuming I finish this post and get off the couch). I’m pretty proud of that! It has certainly taken resolve on my part, but I’ve found that it’s not that hard as long as I plan activity into every day. If I don’t have a dedicated portion of the day to go for a walk or exercise, I make sure to spend 10 minutes here and there walking around the dining room table or the playroom. If I haven’t gotten my steps before I start tutoring, I pace back and forth in my office between students or if they’re working on something independently. Those steps really add up and it’s heart healthy and lung healthy just to move!
This long streak was only possible because I had a very good winter health-wise. I did get sick twice, but both illnesses were (relatively) mild and I was able to shuffle around the table even on the worst days. I find that if I’m having a harder day health-wise, a reasonable amount of movement goes a long way in making me feel better and creating energy. This exercise goal has improved my stamina overall and I’m thankful for that! I know I’ll break the streak eventually, but hopefully not anytime soon. I’d love to reach a year!
***
Thanks for sticking with me through this long post! If you didn’t get a chance to ask your question, or if my answers raised more questions, feel free to submit one now in the comment section or by email (bvbrighthope@gmail.com). I’d be happy to write another post or answer you directly. Thanks for reading!